Posts Tagged "Red Cross"
Stopping Nosebleeds
Nosebleeds can occur randomly or as a result of an injury. Young children are often affected following activity, colds, or exposure to high altitudes. Nosebleeds are more of an annoyance than a serious injury, most of the time. Nosebleeds happen more during the colder winter months when upper respiratory infections are more frequent, and the temperature and humidity fluctuate more dramatically. Though, if there’s profuse or prolonged bleeding, they can be dangerous and a doctor needs to be consulted. Leaders, camp counselors, and parents should always be aware if they’re supervising a child with a history of being prone to getting nosebleeds. Don’t be afraid to ask parents about their child’s medical history before going camping or taking trips away from your usual meeting place.
The most common cause of nosebleeds is drying of the nasal membranes and this can be prevented with proper lubrication of the nasal passages and not picking nose. 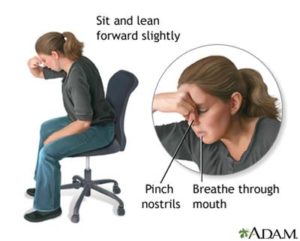
Stopping a Nosebleed
- Have the affected person remain quiet and lean forward slightly with the head tilted forward. Leaning back or tilting the head back allows the blood to run back into your sinuses and throat and can cause gagging or inhaling the blood.
- Pinch the nostrils together with slight pressure. If there’s a good amount of blood, you may want to pack the nostrils lightly and then pinch. Hold for at least 5 minutes.
- Sometimes a cold wet towel, applied to the face, can help to stop the bleeding.
For more, consult the American Red Cross.
Read MoreBasic Wound Care
It is important to be able to identify a wound and care for it. Accidents are common, especially when participating in outdoor activities. While all serious injuries should be checked out by a doctor or other health care professional, leaders and camp counselors should know basic wound care to attend to an injury between the accident site and a trip to a medic. Wounds are subject to infection and bleeding, so attention is required. A wound is defined as a break in the skin or mucous membrane. It is caused by force and usually extends into the underlying tissue. Wounds may be classified into four types:
- Abrasions, made by rubbing or scraping. Floor burns or scuff burns, although called burns, are actually wounds.
- Incised wounds, sharp cuts that tend to bleed freely.
- Lacerated wounds, jagged or irregular wounds, often associated with much tissue damage.
- Puncture wounds. A tack, run through the skin, makes a typical, small puncture wound.
Caring for wounds in which bleeding is not severe is easily done. All adults working with children should know the basic steps.
- Wash your hands thoroughly with clean water and soap.
- Cleanse the injury thoroughly, using plain soap and boiled water cooled to room temperature or clean running tap water and soap.
- Apply the soap and water with a sterile dressing.
- Apply a dry sterile or clean dressing, and bandage it snugly into place.
- See a doctor promptly if evidence of infection appears.
For wounds in which bleeding is server, the objective is to stop the bleeding at once. Always stop the bleeding with pressure directly over the wound with a cloth, if possible. Loss of over a quart of blood may be serious, especially in young children, the aged, and debilitated.
- Direct pressure. Use a clean cloth or a part of the clothing in real emergencies. Apply direct pressure directly over the wound. After the bleeding has been controlled, apply additional layers of cloth to form a sufficient covering, then bandage snugly or firmly.
- Pressure to the supplying vessel. Use the heel of your hand to press the supplying vessel against the underlying bone. Such pressure causes the bleeding to diminish, but doesn’t stop it entirely.
Here are some other tips when dealing with all kinds of wounds:
- If an extremity is involved, elevate it, using pillows or substitutes.
- If there is a delay getting professional medical care, make sure to give the injured person plenty of water if they’re thirsty. You want to make sure they’re properly hydrated. Do not give alcoholic drinks, or give water if there is a penetrating wound of the abdomen or lower chest.
For more, consult the American Red Cross.
Read MoreCaring for Hypothermia
Sometimes, despite your best efforts to prevent hypothermia, symptoms can present themselves anyway, especially in small children. Remember that hypothermia is a big deal – it’s a medical emergency that requires immediate attention by a medical professional. Once you’ve identified hypothermia symptoms, call 9-1-1 or the local emergency number and follow these steps immediately.
- Get out of the water and get to a warm place.
- Remove wet clothing.
- Gradually rewarm your body by wrapping yourself in blankets or putting on dry clothes.
- Cover your head to prevent further heat loss.
- Be careful not to rewarm yourself too quickly. Rapid rewarming can cause dangerous heart rhythms.
- Drink warm nonalcoholic and decaffeinated liquids.
- If you’re caring for someone else and they are unconscious, monitor their breathing and pulse. Be prepared to give rescue breathing or CPR.
For more, read Basic Water Rescue, a booklet published by the American Red Cross.
Identifying Hypothermia
If you’ve been unable to prevent hypothermia, there are some telltale signs for identifying hypothermia. Usually if a member of your group is complaining that they’re cold, be sure to check their temperature. If their temperature is below 96° Some of the signs to look for are:
- Confusion or sleepiness.
- Slowed, slurred speech, or shallow breathing.
- Weak pulse; low blood pressure.
- A change in behavior during cold weather or a change in the way a person looks.
- Excess shivering or no shivering; stiffness in the arms or legs.
- Poor control over body movements or slow reactions.
For more, read Basic Water Rescue, a booklet published by the American Red Cross.
Preventing Hypothermia
Hypothermia doesn’t just happen in the winter or in cold water. Hypothermia can occur in water that’s 70 degrees, so you need to be aware of hypothermia even when enjoying spring and summer water activities. Know how to protect your troop from hypothermia by:
- Always wearing a U.S. Coast Guard-approved life jacket while boating on cold water. A life jacket not only provides flotation, but it also helps the person wearing it to conserve body heat.
- Wearing layers of insulated clothes that keep you warm even while wet, such as clothing made from wool or containing polypropylene or capilene.
- Wearing a wet suit or dry suit during aquatic activities.
- Wearing a hat. Body heat is quickly lost through the head.
For more, read Basic Water Rescue, a booklet published by the American Red Cross.
